Day 3 Highlights from the ADA’s 80th Scientific Sessions
By Eliza SkolerJimmy McDermott
 By Eliza Skoler, Jimmy McDermott, Matthew Garza, Divya Gopisetty, Frida Velcani, and Karena Yan
By Eliza Skoler, Jimmy McDermott, Matthew Garza, Divya Gopisetty, Frida Velcani, and Karena Yan
Check out the third day highlights from ADA’s virtual 80th Scientific Sessions – including new insights on off label use in type 1 diabetes, type 2 diabetes remission, DIY closed loop, DSMES, and more!
Day three of ADA’s Scientific Sessions brought incredibly interesting research, and found us settling into the new virtual format. You can read our highlights from day one here, and from day two here.
Click to jump down to a section:
-
Metformin, GLP-1 agonists, and SGLT-2 inhibitors in Type 1 Diabetes
-
What Therapies Are Best for People with Type 2 Diabetes at Risk of Heart Disease?
-
Real World Stories: Supporting People at Different Stages of Diabetes
-
Diabetes Self-Management Education and Support (DSMES) 2020 Consensus Report Recommendations
Metformin, GLP-1 agonists, and SGLT-2 inhibitors in Type 1 Diabetes
UCSD’s Dr. Jeremy Pettus moderated a session with three expert presenters from across the world: Dr. Irene Hramiak (Western University), Dr. Tina Vilsboll (Steno Diabetes Center Copenhagen), and Dr. Chantal Mathieu (University Hospital Gasthuisberg Leuven).
 Dr. Hramiak kicked things off discussing the current challenges and risks of insulin therapy, including hypoglycemia, weight gain, glucose variability, and diabetic ketoacidosis (DKA). According to data from the T1D Exchange, average A1C levels have not improved in the last decade, and adolescents continue to be a difficult group for glycemic management, despite increased use of pumps and continuous glucose monitors (CGM). How can adjunctive therapies (added to insulin) help?
Dr. Hramiak kicked things off discussing the current challenges and risks of insulin therapy, including hypoglycemia, weight gain, glucose variability, and diabetic ketoacidosis (DKA). According to data from the T1D Exchange, average A1C levels have not improved in the last decade, and adolescents continue to be a difficult group for glycemic management, despite increased use of pumps and continuous glucose monitors (CGM). How can adjunctive therapies (added to insulin) help?
The REMOVAL study looked at the effects of metformin in people with type 1 diabetes (40 years of age or older). Over three years, participants taking metformin saw the following benefits compared to those taking a placebo: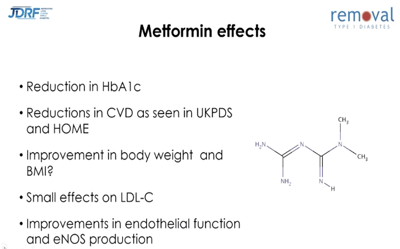
-
A decrease in A1C of 0.13 percentage points
-
A reduction in insulin dose by 1.2 units
-
No change in the rate of minor or severe hypoglycemia
-
From a baseline body weight of 193 lbs (87.7 kg), a weight loss of 2.6 lbs (1.17 kg)
-
A reduction in LDL (“bad”) cholesterol by 0.13 mmol/L (5 mg/dL)
These data suggest that metformin did not have a clinically meaningful impact on glycemic management but may improve cardiovascular health in adults with type 1 diabetes. That’s disappointing, but something we’ve all wondered for years – now we know!
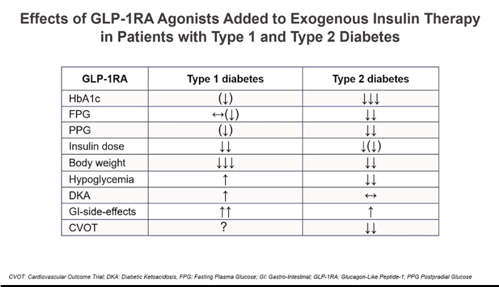
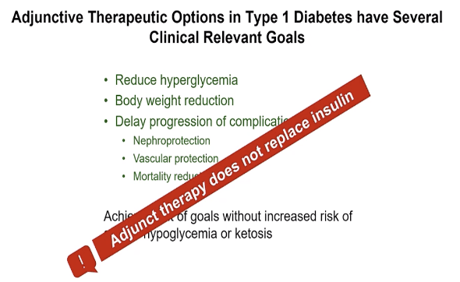 Dr. Vilsboll continued the conversation by discussing GLP-1 agonists for type 1 diabetes. She reminded that adjunctive therapy has several important goals but does not replace insulin – which is the main treatment for people with type 1 diabetes.
Dr. Vilsboll continued the conversation by discussing GLP-1 agonists for type 1 diabetes. She reminded that adjunctive therapy has several important goals but does not replace insulin – which is the main treatment for people with type 1 diabetes.
Dr. Vilsboll provided an overview of the effect of GLP-1 drugs in the pancreas (on insulin-producing beta cells), liver, brain, kidneys, and other organs before sharing data from a trial on GLP-1agonists in type 1 diabetes.
The LIRA-1 Study evaluated 24 weeks of GLP-1 agonist use in people with type 1 diabetes and excess weight and found that GLP-1 treatment:
-
Did not have a statistically significant (meaningful) reduction in A1C compared to placebo.
-
Reduced body weight by 13.4 lbs (6.1 kg) compared to placebo (from a baseline of about 205 lbs, or 93 kg).
-
Increased gastrointestinal side effects (nausea, diarrhea).
-
Did not decrease the amount of bolus insulin required but reduced basal insulin by about five to six units per day.
The ADJUNCT trial was the longest such trial, involving 1,400 people with type 1 diabetes with an A1C between 7%-10%. In this trial, participants taking GLP-1 agonists experienced:
-
A clinically significant reduction in A1C of 0.54 percentage points compared to a baseline of 8.2% after 52 weeks.
-
A reduction in body weight that correlated with the dose of GLP-1 agonist: 10.8 lbs (4.9 kg) of weight loss with a 1.8 mg dose of GLP-1 agonist; 7.9 lbs (3.6 kg) with a 1.2 mg dose; and 4.9 lbs (2.2 kg) with a 0.6 mg dose.
-
An increased rate of symptomatic hypoglycemia, but no increase in severe hypoglycemia or DKA.
In a more recent trial, MAG1C, researchers examined the use of GLP-1 agonist exenatide (Byetta) over 26 weeks in adults with type 1 diabetes. Researchers found that compared to placebo, the GLP-1 agonist did not decrease A1C but did decrease insulin dose and body weight. Researchers concluded that the GLP-1 agonist does not have a future as an add-on treatment to insulin in type 1 diabetes. We are not certain this is the correct answer, because it seems like TIR would’ve been useful to measure – but, there’s no fighting city hall.
The session concluded with Dr. Chantal Mathieu discussing the role of SLGT-2 inhibitors in people with type 1 diabetes. She pointed to three main trials: DEPICT with Farxiga, InTANDEM with Zynquista, and EASE with Jardiance.
Compared to placebo, participants taking Farxiga (either 5mg or 10mg dose) experienced:
-
Approximately a 0.45 percentage point drop in A1C by 24 weeks, and 0.2 to 0.3 percentage point decrease in A1C after 52 weeks.
- A time in range increase of about 10% – a gain of almost two more hours of time in range per day
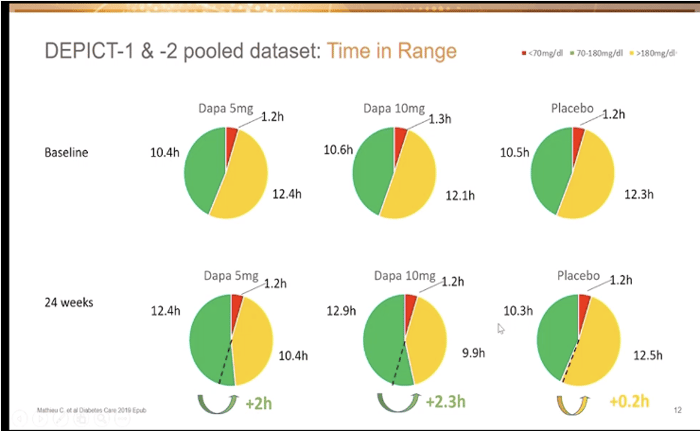
-
A 10% decrease in both basal and bolus insulin.
-
A decrease in body weight of about 5.5 lbs (2.5 kg) with a 5mg dose, and about 7.7 lbs (3.5 kg) with a 10mg dose (from a baseline of 179 lbs, or 81 kg).
-
An increased risk of genital infection and urinary tract infections.
-
No increase in hypoglycemia.
-
An increased risk of DKA that rises with a larger dose.
The inTandem trial also showed a drop in A1C: after 24 weeks, participants taking Zynquista experienced a 0.5 percentage point drop in A1C compared to those taking placebo. Time in range also increased with Zynquista. There was a 77-minute increase in time in range with the 200 mg dose, and almost a three-hour increase for people taking the 400mg dose. The increased risks of DKA and genital infections were also observed in this trial.
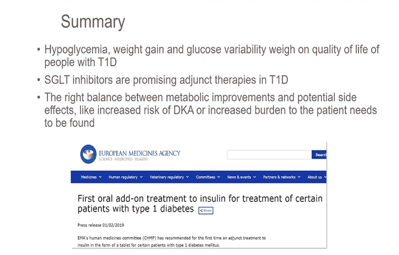 The EASE trial provided evidence that supported the effects of SGLT-2 inhibitors on the reduction of A1C – about 0.3-0.4 percentage points after 52 weeks. This study also used a much lower dose of 2.5 mg, which offered an intermediate effect – lowering A1C by about 0.2 percentage points and reducing body weight by 4 lbs (1.8 kg). Interestingly, there was no difference in DKA with the 2.5 mg dose compared to placebo.
The EASE trial provided evidence that supported the effects of SGLT-2 inhibitors on the reduction of A1C – about 0.3-0.4 percentage points after 52 weeks. This study also used a much lower dose of 2.5 mg, which offered an intermediate effect – lowering A1C by about 0.2 percentage points and reducing body weight by 4 lbs (1.8 kg). Interestingly, there was no difference in DKA with the 2.5 mg dose compared to placebo.
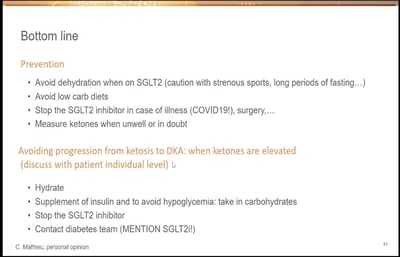
Dr. Mathieu concluded by sharing her “bottom line” on the use of SGLT-2 inhibitors in type 1 diabetes and preventing DKA.
 To learn more about off-label drugs in type 1 diabetes, check out this article from Kerri Sparling.
To learn more about off-label drugs in type 1 diabetes, check out this article from Kerri Sparling.
Lifestyle Interventions for Type 2 Diabetes Remission
In a fascinating session on type 2 diabetes remission, several leaders in the field introduced data on how specific lifestyle interventions (diet and exercise) may help put type 2 diabetes into remission.
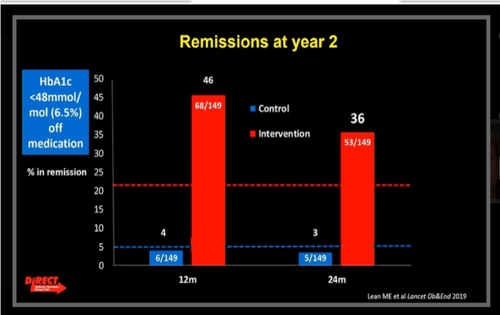
Alison Barnes presented data from the DiRECT trial, which focused on low-calorie diets (LCD). The trial compared an intervention group on an LCD (between 800-900 calories per day) to a control group receiving typical diabetes care. Remission was defined as achieving an A1C below 6.5% and stopping all diabetes medications. Results from the DiRECT trial were promising:
-
At one year: 4% remission in control group and 46% remission in the intervention group.
-
At two years: 3% remission in control group and 36% remission in the intervention group.
-
64% of participants who lost more than 22 lbs (10 kg) were in remission at two years.
-
The intervention group dropped from 75% of participants on diabetes medications at baseline to 40% at two years (compared to 77% at baseline and up to 84% in the control group).
-
Average A1C decreased by 0.6 percentage points in the intervention group at 2 years.
 We thoroughly recommend Dr. Roy Taylor’s book Life Without Diabetes: The Definitive Guide to Understanding and Reversing Type 2 Diabetes – he provides a major connection to the DiRECT trial.
We thoroughly recommend Dr. Roy Taylor’s book Life Without Diabetes: The Definitive Guide to Understanding and Reversing Type 2 Diabetes – he provides a major connection to the DiRECT trial.
Next Dr. William Yancy spoke on low-carbohydrate diets (classified as less than 130 g carbs per day, with no overall calorie restrictions). In an analysis that compared the effects of nine different diets on glycemic outcomes in type 2 diabetes, the low-carb diet was ranked as the most effective dietary approach for lowering A1C.
Finally, Dr. Kristian Karstoft presented the U-TURN study on how exercise alone, or exercise and diet, may play a role in type 2 diabetes remission. U-TURN had two groups, one receiving standard care and one receiving intensive lifestyle intervention, which included diet and exercise components.
-
After 12 months, 37% of participants in the intervention group stopped using glucose-lowering medication and maintained glucose levels below the criteria for type 2 diabetes (effectively achieving remission).
-
Of the participants who achieved remission, the majority of them came from the group that consistently exercised the most.
Parent Perspectives on DIY Closed-Loop
An observational study on Loop, a do-it-yourself (DIY) automated insulin delivery system (AID), used focus groups to gather the attitudes and experiences of parents and children using Loop. The study followed people using an AID system, continuous glucose monitor (CGM) readings, and a communications bridge device, called “RileyLink.”
Overall, parents felt that Loop had a positive impact on their family’s lives. They reported the following outcomes:
-
Improvements in emotional health as a result of a greater sense of security and normalcy, increased quality of life, and decreased parental stress.
-
Improvements in other areas of life, including management of children’s diabetes at school, quality of sleep, confidence in caregivers, and children’s ability to explore extracurriculars without supervision.
Dr. Anastasia Albanese-O’Neill presented survey results on what parents expect of school and diabetes camp staff to help their children manage their DIY closed-loop system. School nurses were also surveyed on their opinions regarding DIY. Here are some highlights:
-
29% of parents expect that school staff will assist children with delivering a bolus.
-
Expectations of diabetes camp staff were lower than school staff – 23% of parents expect school staff to assist with carbohydrate counting and timing of bolus, while only 13% of parents expect diabetes camp staff to do those things.
-
Though 46% of school nurses had never heard of DIY before participating in the survey, 33% of them agreed that school staff should help students using DIY who cannot manage it independently.
This suggests a need for training on DIY and diabetes technology for school and camp staff.
What Therapies Are Best for People with Type 2 Diabetes at Risk of Heart Disease?
The world of diabetes is now focusing more than ever on preventing diabetes-related health complications. Not only is the treatment of diabetes about blood sugar (measured by A1C or time in range), but it is also about heart health, kidney health, and so much more. In 2019, data from large trials showed that GLP-1 agonists and SGLT-2 inhibitors have heart and kidney protection benefits.
As such, experts strongly emphasized using GLP-1 or SGLT-2 drugs for individuals at high-risk for heart attack, stroke, heart failure, or chronic kidney disease. They also named that GLP-1 and SGLT-2 therapies should become more accessible and affordable to people living with diabetes.
Studies have not yet evaluated the heart and kidney health benefits of metformin, compared to those of GLP-1s and SGLT-2s. However, trials have shown that metformin helps lower blood glucose and body weight, comes with a low risk of hypoglycemia, and is cost-effective.
If your healthcare professional has not brought up additional therapy options for you, we recommend you ask them to read this article and discuss your options.
Real World Stories: Supporting People at Different Stages of Diabetes
Dr. Neesha Ramchandani presented her work on young adults living with diabetes (ages 18 to 30). Through interviews, she found four main challenges: finding a balance between diabetes and life, feeling in control of diabetes, navigating the hidden burden of diabetes within their social circles, and wanting a better connection with their diabetes healthcare professional. One participant said, “Diabetes is like having a full-time job… you can’t 100% turn off. It always has to be a part of your thought process.” diaTribe has resources for teens here.
We then heard from Dr. Della Connor and Dr. Gary Rothenberg on the need to care for people who are living with diabetes post-kidney transplants and post-amputations. In all three talks, the experts emphasized the need to:
-
Build trust and comfort between people with diabetes and healthcare professionals.
-
Incorporate perspectives based on gender, race, and ethnicity into care.
-
Recognize the importance of a team approach, including care-partners.
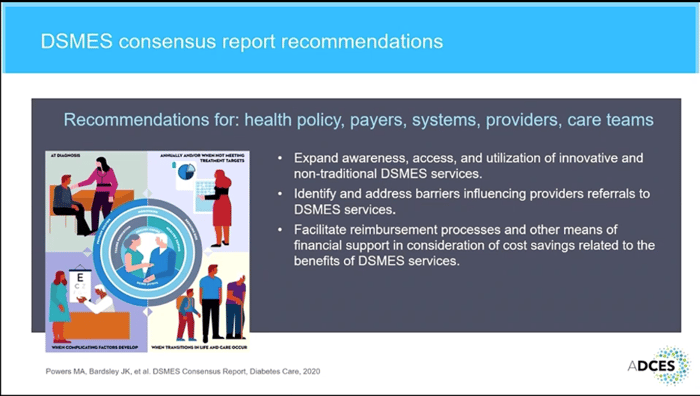
Diabetes Self-Management Education and Support (DSMES) 2020 Consensus Report Recommendations
A group of educators made a strong case for the greater use of diabetes self-management education and support (DSMES). The benefits are many, including improvements in clinical, behavioral, and psychosocial outcomes, and greater diabetes knowledge and self-care behaviors. Dr. Margaret Powers stressed that compared to other treatments prescribed by healthcare professionals, DSMES and medical nutrition therapy produce few to no negative side effects for people with diabetes and are low cost.
.png)
The experts discussed low DSMES participation rates across the nation and the factors that reduce referrals to diabetes education. Evidence shows that less than 5% of people newly diagnosed with diabetes who have Medicare insurance, and 6.8% of privately insured people with diabetes, have used DSMES services. The 2020 DSMES Consensus Report was created to address these concerns by outlining steps healthcare professionals can take to help people access DSMES services. The report recommends that healthcare professionals make referrals and encourage participation in DSMES at four critical times in someone’s diabetes journey: (1) diagnosis, (2) annually or when not meeting treatment targets, (3) when complicating factors develop, and (4) when transitions in life and care occur. It also suggests that awareness of, and access to, DSMES must be expanded (culturally and geographically), and financial support should be provided for use of DSMES services..png)