How CGM Changed the Life of Someone Without Diabetes
 By Jody Maryniak
By Jody Maryniak
Key lessons learned from my ongoing battle with adrenal insufficiency, and the unexpected role of diabetes technology.
It’s easy to write off a lot of symptoms when you’re a new mother of twins. Mind-numbing fatigue and brain fog? That’s to be expected…right? But as my twins turned one, I regained all my lost pregnancy weight despite regular exercise, and I regularly woke up drenched in sweat. It was hard to ignore the fact that there might be something else going on.
A long series of appointments ensued, filled with blood draws, MRIs, and skeptical doctors. Extensive tests revealed that I was missing a significant portion of my pituitary: a tiny, pea-sized gland in your brain that releases several vital hormones. Despite a diagnosis of hypopituitarism and an appropriate treatment plan that addressed my night sweats and weight gain, I still couldn’t shake the overwhelming fatigue.
Unfortunately, my doctor didn’t feel this warranted treatment. Over the course of the next four years, I was told repeatedly that I was “fine” and that “maybe you’re bored” (yes, my doctor actually told me that - although how any working mother of twins can be bored, I’m not sure!).
While starting to feel like maybe it was all “in my head,” it became hard to ignore the peak in symptoms this past spring and summer. I was often nauseous, dizzy, and felt like my head was spinning. I was dragging myself out of and into bed each day. At doctor appointments, I learned my weight dropped and my blood pressure readings were alarmingly low. Then, perhaps fortuitously, I had routine lab work ordered as part of my annual physical. The venous lab work came back with a non-fasting blood glucose reading of 51 mg/dl!
My family doctor and my husband Matt, a consultant in the field of diabetes and metabolic medicine, assured me that couldn’t be correct. A re-test, however, showed another non-fasting blood glucose reading of 60 mg/dL. When my endocrinologist brushed these results off and told me to “pretend you never saw them,” I knew it was time to advocate for myself and find a new endocrinologist.
Endocrinologist #2 also brushed off my symptoms and low blood pressure and low glucose readings, stating that “they aren’t life-threatening.” Maybe not, but what if I had a severe hypoglycemic episode while driving with my children in the car?
Enter Endocrinologist #3. For the first time, I felt like someone listened and took my symptoms seriously. She looked at my very real numbers and felt certain this was an actual, serious medical problem. Comprehensive testing revealed orthostatic hypotension, a common symptom of low cortisol and indicator of adrenal insufficiency. She immediately prescribed treatments for my adrenal insufficiency, and my health did improve significantly. Despite these improvements, though, I continued to have bouts of dizziness and shakiness along with blurred vision and brain fog.
 Now equipped with a blood glucose meter, I did random fingersticks when feeling shaky. I noticed that after exercise, my blood sugar would often be in the 60s. Thinking that it was only occurring occasionally, my husband mentioned that it might be helpful to use a continuous glucose monitor (CGM) to get a better idea of my blood glucose patterns.
Now equipped with a blood glucose meter, I did random fingersticks when feeling shaky. I noticed that after exercise, my blood sugar would often be in the 60s. Thinking that it was only occurring occasionally, my husband mentioned that it might be helpful to use a continuous glucose monitor (CGM) to get a better idea of my blood glucose patterns.
I then had the frustrating experience of realizing that insurance would not cover a CGM for someone who is not a person with type 1 diabetes. (Editor’s Note: it’s often challenging even for people with type 1 diabetes to get a CGM covered by insurance, and Medicare does not cover personal CGM at all.) It was hard to accept that a technology that could really help me understand my condition was just beyond my reach. Eventually, through Matt’s connections with the diabetes community, I was grateful to be able to borrow a loaner Dexcom G4 CGM.
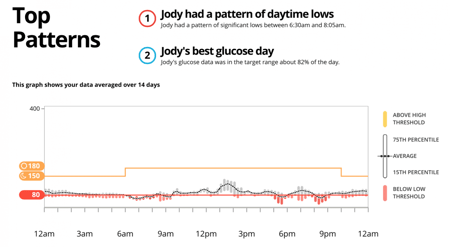
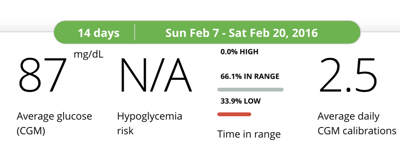 The week that I wore the CGM was eye-opening. Over the course of the week, I was in a hypoglycemic state 34% of the time. My blood glucose levels were extremely unpredictable and variable, whether or not I was fasting. After exercise, my readings would drop below levels measurable by the CGM (<40mg/dl). They’d often drop overnight and in the early morning too. It was downright scary, but informative. All of those symptoms I’d been trying to ignore were really hypoglycemic symptoms. Without the CGM, we never would have been able to collect all of this data.
The week that I wore the CGM was eye-opening. Over the course of the week, I was in a hypoglycemic state 34% of the time. My blood glucose levels were extremely unpredictable and variable, whether or not I was fasting. After exercise, my readings would drop below levels measurable by the CGM (<40mg/dl). They’d often drop overnight and in the early morning too. It was downright scary, but informative. All of those symptoms I’d been trying to ignore were really hypoglycemic symptoms. Without the CGM, we never would have been able to collect all of this data.
Now that we have this data, we’re embarking on a quest to determine the cause. It’s frustrating to think about all of the wasted time with my previous endocrinologists, but I’m thankful that my new endocrinologist is taking this seriously and consulting with other prominent doctors for possible causes. She routinely assures me that “we’ll get to the bottom of this!”
The thing about having rare medical diagnoses is that it can be hard to find support - online or in person. I have found a few online forums for others with my diagnoses and many people have detailed similar, years-long struggles to get proper diagnoses. It’s also easy for doctors, friends, and family to brush off your symptoms and concerns. Aren’t we all tired? Don’t we all get a bit shaky and “hangry” when we need to eat? Don’t people want low blood pressure and low blood sugar? Turns out there is definitely such a thing as too low!
While the past five years have been difficult, I’ve learned a few things:
-
Listen to your body and be your own best advocate. Be persistent when something doesn’t feel right!
-
Just because a doctor works at a prestigious clinic or hospital, doesn’t mean they’re the best fit for you. Bedside manner and feeling like you’ve been heard can make a world of difference.
-
There is some amazing technology in the field of medicine (like CGM) and we should advocate to make them available to everyone with an appropriate diagnosis.
Bio
Jody is a speech-language pathologist who works with K-12 students in a public school district and teaches communication disorders courses at a local university. In her (limited) spare time, she enjoys baking, traveling, and yoga. She currently lives outside of Philadelphia, Pennsylvania with her husband Matt and twin daughters.
Editor’s Note: We heard about Jody’s story and were inspired by not only her perseverance in the face of less-than-supportive healthcare teams, but also the ways in which diabetes technology helped diagnose her potentially life-threatening case of adrenal insufficiency. She explained her story to us as one in which the diabetes community “came to the rescue,” and while she does not have diabetes herself, we hope her experience resonates with our readers on the importance of patient advocacy and the innovations in diabetes technology today.







