Benefits of Time in Range: New Study Shows Cost Savings

By Eliza Skoler and Albert Cai
A new paper suggests that as people with diabetes increase their time in range, healthcare costs decrease
IQVIA, a healthcare consulting firm, published a 22-page paper describing the limitations of A1C and the potential financial benefits of improving time in range, the time a person spends with blood glucose levels between 70-180 mg/dl. The paper was sponsored by Lilly Diabetes.
The paper predicts that if the average time in range for people with diabetes in the US increases to 70% or 80%, healthcare costs will be reduced. The savings could be up to $9.7 billion for the US healthcare system over ten years if the average time in range for people with diabetes is increased to 80%.
The graphic below shows how much money is saved over ten years just by reducing hypoglycemic (low blood sugar) events in people with type 1 diabetes. Other costs saving would likely come from a reduction in diabetes-related complications. Studies (Diabetes Care 2019, Diabetes Care 2018) have suggested that greater time in range is associated with a lower risk of health complications.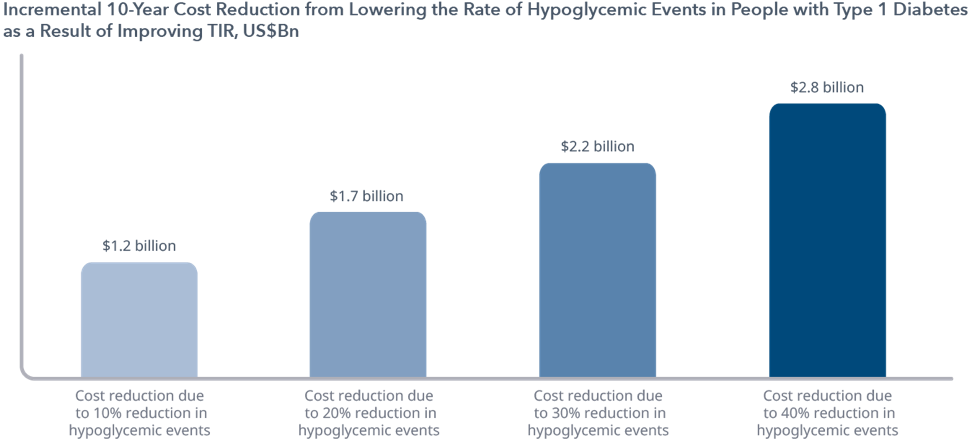
Unsurprisingly, the biggest reductions in healthcare costs were seen in people with high baseline A1C. While a 5% increase in time in range for a person with an A1C under 7% would save only $20 over ten years, the same 5% increase in time in range for a person with an A1C over 8% would lead to $1,470 in savings over ten years – mostly due to a greater reduction in the risk of diabetes-related complications. This means that to get the greatest health and cost benefits, it is essential to bring time in range practices to people who are most struggling to manage their blood glucose.
To calculate the effects of improving time in range, the study assumed an average time in range for people in the US of 58% (type 1 and type 2 diabetes). This 58% came from a 2019 review of four major CGM studies. However, these four studies were done at top diabetes centers and the participants had relatively low A1Cs (~7.5%). Additionally, the majority of people with type 1 diabetes and almost everyone with type 2 diabetes still don’t have access to CGMs. In other words, the actual population average is likely much lower than 58% time in range and the $9.7 billion calculated in cost savings would actually be much higher if the population’s time in range reached 80%.
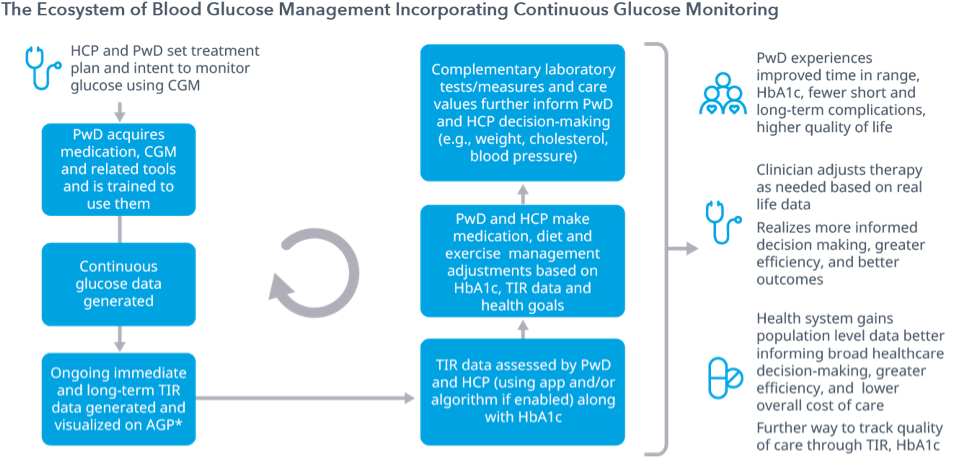
IQVIA provides several reasons why CGM should be used to support blood glucose management in people with diabetes:
-
A person with diabetes can understand how variables like food, exercise, and sleep habits affect blood glucose and can use that information to improve decisions and outcomes.
-
Healthcare professionals can provide more individualized care to support people with diabetes.
-
The healthcare system will save money on diabetes care.
The illustration below outlines how CGM can be used to monitor blood glucose and guide shared decision making for a healthcare professional (HCP) and person with diabetes (PwD).
The last eight pages of the paper discuss how time in range can become more commonly used, asking policymakers, healthcare professionals, and people with diabetes to drive the time in range movement forward. IQVIA’s ideas include:
-
promoting CGM to help people measure and understand time in range;
-
educating healthcare professionals and people with diabetes about the health benefits of time in range; and,
-
tackling affordability and access issues to make sure all people with diabetes (or even prediabetes) can use CGM.
This paper not only emphasizes the importance of time in range for well-being but also highlights time in range as a public policy matter. While there is clearly much work to be done, this study is an important step in underscoring the need to bring CGM and time in range to more people.