Our Preview of the American Diabetes Association Scientific Sessions

By Kelly Close, Alexander Wolf, Adam Brown, and Manu Venkat
Twitter Summary: We discuss our top-anticipated sessions at the @AmDiabetesAssn #2015ADA Conference in Boston – heart safety, combo drugs, #artificialpancreas + more!
The American Diabetes Association's 75th Annual Scientific Sessions kicks off tomorrow in Boston, marking one of the biggest and most anticipated weeks of the year in diabetes. We at diaTribe will be on the scene covering the conference – follow us on Twitter at @diaTribeNews for daily updates!
 So what is happening this year at ADA? Out of the thousands of amazing posters, presentations, and meetings, we’ve identified a few key sessions we’re particularly excited about at diaTribe:
So what is happening this year at ADA? Out of the thousands of amazing posters, presentations, and meetings, we’ve identified a few key sessions we’re particularly excited about at diaTribe:
BIG PICTURE
Results from Major Cardiovascular Outcomes Trials
One major highlight of ADA will be the results of two big heart safety outcomes trials called TECOS and ELIXA. These trials observed patients using DPP-4 inhibitor and GLP-1 agonist drugs (Januvia and Lyxumia, respectively) over long periods of time in order to examine their effects on cardiovascular events like heart attacks and strokes. As these two drug classes are commonly used and offer many benefits for patients with diabetes, it’s vital that we as a community understand if and how they impact heart disease. Our own Kelly Close recently spoke to the FDA about the need to more clearly establish the heart safety implications of these drugs, and we look forward to learning more at ADA.
FLAT-SUGAR Trial Results on Glycemic Variability
 Renowned expert endocrinologist Dr. Irl Hirsch (University of Washington) will be presenting results from the FLAT-SUGAR study, which examined methods of measuring glycemic variability independent of A1c. Right now, the FDA approves drugs based on their effect on lowering A1c, and A1c is also the typical gold standard used by health care providers to gauge their patients’ glucose control. However, A1c provides an incomplete picture of blood glucose management; the measurement roughly averages glucose levels over a three-month period, meaning that two patients with the same A1c may actually have very different levels of control (i.e., one patient may spend the majority of time in range, whereas another patient could have frequent extreme episodes of hypoglycemia and hyperglycemia, and both could average out to the same A1c value).
Renowned expert endocrinologist Dr. Irl Hirsch (University of Washington) will be presenting results from the FLAT-SUGAR study, which examined methods of measuring glycemic variability independent of A1c. Right now, the FDA approves drugs based on their effect on lowering A1c, and A1c is also the typical gold standard used by health care providers to gauge their patients’ glucose control. However, A1c provides an incomplete picture of blood glucose management; the measurement roughly averages glucose levels over a three-month period, meaning that two patients with the same A1c may actually have very different levels of control (i.e., one patient may spend the majority of time in range, whereas another patient could have frequent extreme episodes of hypoglycemia and hyperglycemia, and both could average out to the same A1c value).
Some researchers have hypothesized that this kind of glycemic variability – oscillating between low and high blood sugars on a regular basis – may in and of itself have harmful effects on one’s health. The primary goal of the FLAT-SUGAR study is to see if it is feasible to reduce glycemic variability without changing A1c. This study is a pilot that should set the foundation for future trials that will investigate the effects of glycemic variability, independent of A1c, on diabetes complications and overall health.
On another note, Dr. Hirsch will also be presenting what is expected to be a very passionate, no holds barred talk on the rising costs of insulin, particularly for those without insurance who are most vulnerable to increases in wholesale drug costs. For more background on this topic, see our recent learning curve here.
DEVICES
Moving Towards a Closed-Loop System
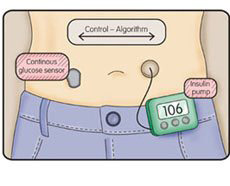 On the technology front, one of the most highly hyped sessions will provide an outstanding overview of the worldwide status of artificial pancreas research, featuring presentations from some of the top leaders in the field. This includes representatives from the DREAM Consortium (recently licensed by Medtronic), the Bionic Pancreas, the UVA DiAs Sytem, and more. In particular, we are excited to hear Dr. Steven Russell (Massachusetts General Hospital) present the results from Bionic Pancreas trials in pre-adolescents, presumably from the team’s 2014 summer camp trials in 6-11 year old kids, as well as updates from Dr. Stacey Anderson (UVA) on the DiAs overnight and 24/7 closed-loop clinical trials.
On the technology front, one of the most highly hyped sessions will provide an outstanding overview of the worldwide status of artificial pancreas research, featuring presentations from some of the top leaders in the field. This includes representatives from the DREAM Consortium (recently licensed by Medtronic), the Bionic Pancreas, the UVA DiAs Sytem, and more. In particular, we are excited to hear Dr. Steven Russell (Massachusetts General Hospital) present the results from Bionic Pancreas trials in pre-adolescents, presumably from the team’s 2014 summer camp trials in 6-11 year old kids, as well as updates from Dr. Stacey Anderson (UVA) on the DiAs overnight and 24/7 closed-loop clinical trials.
More broadly, as Adam Brown recently described in an interview with TuDiabetes, this year’s conference will focus not only on the technology itself, but also how patients are actually using it. The sessions will hopefully address questions such as, “What’s the burden on people?” and, “What’s it like to use an artificial pancreas?” At ATTD in Paris, there was an phenomenal session on the “Human Side of the Artificial Pancreas” – a follow-up session will be occurring at ADA as well, continuing the discussion on bringing artificial pancreas technology into the people’s daily lives.
DRUGS
An Implantable GLP-1 Agonist Pump
 Intarcia Therapeutics will be presenting much awaited data from the FREEDOM-1 phase 3 trials studying ITCA-650, a small implantable device used to treat type 2 diabetes. The tiny device is implanted under the skin for six months or one year and continuously releases exenatide (a GLP-1 agonist) through a small mini-pump. Preliminary results released this January demonstrated that for the overall study population, the average drop in A1c using ITCA-650 was 1.4%-1.5% after 39 weeks (from a starting A1c of 8.4%). Additionally, within a group of patients with a very high starting A1c of 10.8%, the average drop in A1c was an impressive 3.4% after 24 weeks. We look forward to seeing more extensive data on this highly innovative product this Monday at ADA.
Intarcia Therapeutics will be presenting much awaited data from the FREEDOM-1 phase 3 trials studying ITCA-650, a small implantable device used to treat type 2 diabetes. The tiny device is implanted under the skin for six months or one year and continuously releases exenatide (a GLP-1 agonist) through a small mini-pump. Preliminary results released this January demonstrated that for the overall study population, the average drop in A1c using ITCA-650 was 1.4%-1.5% after 39 weeks (from a starting A1c of 8.4%). Additionally, within a group of patients with a very high starting A1c of 10.8%, the average drop in A1c was an impressive 3.4% after 24 weeks. We look forward to seeing more extensive data on this highly innovative product this Monday at ADA.
Basal Insulin/ GLP-1 Agonist Combinations
Another ADA session will be focusing on trial results from what is arguably the most exciting class of drug combinations in type 2 diabetes: basal insulin/GLP-1 agonist combinations. Most notably, Dr. John Buse (UNC Chapel Hill) will present full trial results from the DUAL V phase 3 trial for Novo Nordisk’s Xultophy (Tresiba/Victoza), which received European approval last September. This trial compared Xultophy to Lantus in type 2 diabetes, and preliminary results showed that patients on Lantus who switched to Xultophy saw significant reductions in A1c compared to those who stayed on Lantus, as well as a 7 lb relative weight benefit.
Triple Therapy of Type 2 Diabetes Drugs
In a session on SGLT-2 inhibitors chaired by Dr. Silvio Inzucchi (Yale University), we are most looking forward to hearing results from two phase 3 clinical trials by AstraZeneca (ClinicalTrials.gov Identifiers: NCT01646320 and NCT01619059) on a triple therapy approach using the DPP-4 inhibitor Onglyza, the SGLT-2 inhibitor Farxiga, and metformin. If these results are positive, it is likely that AstraZeneca may pursue a triple fixed-dose combination drug using these three ingredients, though they have indicated that an FDA submission of this triple-combination drug would not take place until 2017 at the earliest. The rest of the presentations in this session will reveal more long-term safety and efficacy data for SGLT-2 drugs, which will provide useful information to health care providers prescribing this drug class (as the first SGLT-2 inhibitor, Invokana, was only approved in March, 2013).
While these presentations are focused solely on type 2 diabetes, there may be additional commentary from speakers on off-label use of the drugs in type 1 diabetes, particularly as the FDA has recently issued a safety warning concerning reports of euglycemic diabetic ketoacidosis caused by these drugs.