Newest Updates and Insights in Diabetes Education from ADCES 2020
By Matthew GarzaEliza Skoler
.jpg) By Matthew Garza, Eliza Skoler, Frida Velcani, and Nena Kotsalidis
By Matthew Garza, Eliza Skoler, Frida Velcani, and Nena Kotsalidis
The Association of Diabetes Care and Education Specialists 2020 conference covered the benefits of sleep education for diabetes management, medications that support kidney health, caring for adults with diabetes during COVID-19, and more!
At the incredible virtual Association of Diabetes Care and Education Specialists (ADCES) conference this weekend, experts discussed some of the most important (and current) aspects of diabetes education and care. Read some of our top highlights below and stay tuned for more from the conference soon!
Click to jump down to a section:
-
Sleep education can improve diabetes knowledge and management, and increase motivation for change
-
Treating diabetes and kidney disease: SGLT-2 inhibitor drugs can support kidney health
-
A pharmacist-led collaborative care model improved health metrics for people with type 2 diabetes
Sleep Education Can Improve Diabetes Knowledge and Management, and Increase Motivation for Change
Dr. Abhishek Pandey, a sleep scientist, presented results from the Sleep Integrated with Diabetes Education trial (SLIDE). The study combined sleep health education with a traditional Diabetes Self-Management Education and Support (DSMES) program to examine the relationship between healthy sleep, motivation for change, and type 2 diabetes management. About 30% of people with type 2 diabetes have sleep disorders, compared to 8.2% of people without type 2 diabetes.
Fifty people from an urban area in Florida were randomly assigned to the sleep and diabetes education group or to the traditional diabetes education group. The majority of participants were Black (62%), female (71%), low-income (85% of participants were making less than $20,000 per year), and uninsured (59%). At baseline, only 11% of participants reported “normal” sleep, and 41% of participants said they usually slept for less than six hours each night. The average A1C for the participants was 8.8%.
The study found that people receiving sleep education got up to 2.3 more hours of sleep per night! In the standard group, sleep went down by as much as 1.2 hours. Notably, lower rates of hypoglycemia, hyperglycemia, and hospitalization were seen in the sleep education group. No significant differences in A1C levels were seen between the two groups, though the follow-up period for the study was short; we imagine there may have been differences in time in range. Click here to learn more about the importance of sleep in diabetes by Adam Brown, a person with diabetes and a guru in thinking about sleep.
Furthermore, participants who received “adequate” sleep were most likely to increase their knowledge of diabetes and also show improvements in health. People in the sleep education group who were highly motivated for change improved both their sleep (by 2.4 hours per night), and their diabetes management (average A1C went down by 1.3 percentage points – baseline A1C for the group was not reported). Happily, people in the same group who were less motivated for change still showed more sleep (1.7 more hours per night). Dr. Pandey concluded that integrating “culturally tailored sleep health sessions” into diabetes education programs can help improve both sleep and diabetes management.
What do we know about COVID-19 and diabetes, and what can healthcare teams do to better help adults with diabetes?
Melissa Young, a clinical pharmacist and diabetes educator, shared what researchers know about COVID cases in the United States and around the world. The clinical outcomes of two previous coronaviruses – SARS-CoV and MERS-CoV – showed that diabetes is a known risk factor for severe illness, and hyperglycemia increases risk of death (because high blood glucose levels decrease the strength of the immune system).
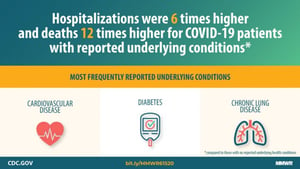 This pattern has also been seen with COVID-19 – chronic conditions, including diabetes, heart disease, lung disease, and high blood pressure all show higher rates of COVID diagnosis and death. In the US about 11% of people have diabetes; however, a May study found that 30% of people diagnosed with COVID also had diabetes. (Image source: CDC)
This pattern has also been seen with COVID-19 – chronic conditions, including diabetes, heart disease, lung disease, and high blood pressure all show higher rates of COVID diagnosis and death. In the US about 11% of people have diabetes; however, a May study found that 30% of people diagnosed with COVID also had diabetes. (Image source: CDC)
At the end of March, a study of more than 7,000 people in the US with COVID-19 found that:
-
24% of people hospitalized had diabetes;
-
32% of people admitted to the intensive care unit had diabetes; and
-
6% of people who were not hospitalized had diabetes.
This risk of more severe outcomes of COVID-19 infection is especially true for people with type 2 diabetes, Ms. Young said – though there is not yet consensus on what is prompting these outcomes.
Dr. Debra Simmons, an endocrinologist at the University of Utah, reminded listeners that even though people over 65 are at higher risk of severe COVID-19 illness (and the highest risk of death due to COVID-19 complications), anyone can be at risk, even if they are not yet 65 years old.
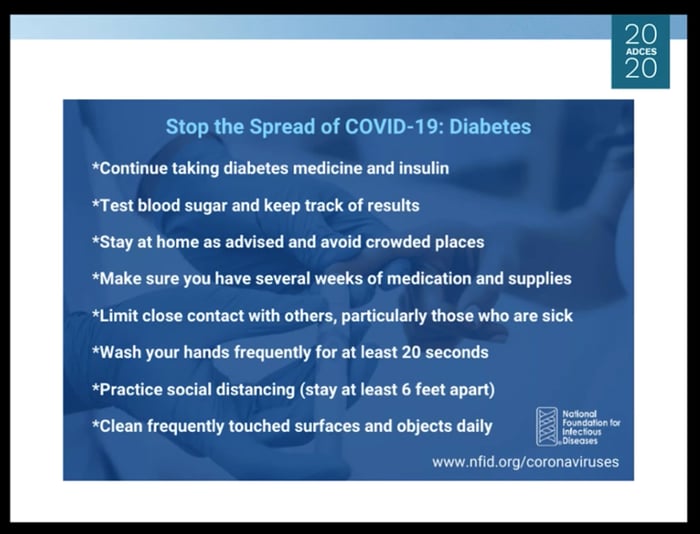
 Dr. Simmons talked about how healthcare professionals can keep people with diabetes safe, emphasizing prevention, education about diabetes management and wellness, and access to urgent care as needed. She suggested that COVID screening questions and education resources be added to every in-person clinical or virtual appointment, and that healthcare professionals talk to people about what to do specifically in case of illness. She also suggested that pharmacies play an even more active role in education, handing out information to people who are at increased risk when they receive their medications and supplies.
Dr. Simmons talked about how healthcare professionals can keep people with diabetes safe, emphasizing prevention, education about diabetes management and wellness, and access to urgent care as needed. She suggested that COVID screening questions and education resources be added to every in-person clinical or virtual appointment, and that healthcare professionals talk to people about what to do specifically in case of illness. She also suggested that pharmacies play an even more active role in education, handing out information to people who are at increased risk when they receive their medications and supplies.
Dr. Simmons noted that it is essential that healthcare professionals and diabetes care and education specialists remind people of a few key things – while some of these may seem intuitive, we are including them as a reminder:
-
There is currently no vaccine for COVID, nor is there a medication that cures COVID. We also know that most vaccines take multiple years to develop.
-
Prevention is essential to keeping people safe – preventing transmission by social distancing and wearing masks is important.
-
People can transmit COVID-19 without knowing it, whether or not they have any symptoms.
-
There are many education resources available through the CDC and the ADA; share these with people with diabetes. Plus, find diaTribe’s many resources at diaTribe.org/covid-19.
-
Help people prepare for their telehealth visits, so that they know what to expect, are comfortable with the technology, and know what to do if they run into technical difficulties.
-
It’s important to get normal vaccines, including flu shots, in a safe environment.
Young mentioned the effects of national emergencies on chronic conditions: a 2017 review of health outcomes after floods and storms found an increase in health complications, including both short-term and long-term diabetes complications. This is something that people with diabetes should know; during this international emergency, please continue to manage your diabetes and take care of your health as much as possible to decrease the risk of complications.
For more resources on COVID-19, click here.
Treating diabetes and kidney disease: SGLT-2 inhibitor drugs can support kidney health
Lourdes Cross, a pharmacist and diabetes care and education specialist, discussed medications that people with diabetes and chronic kidney disease (CKD) can take to support both diabetes health and kidney health. Kidney disease is a long-term condition in which a person’s kidney is damaged and cannot work fully; diabetes is the leading cause of kidney failure. Learn about kidney disease here.
While technically metformin remains the first medication recommended to support diabetes management for people with type 2 diabetes and kidney disease, Cross showed remarkable data indicating where chronic kidney disease prevention may be possible. Notably, research supports the use of SGLT-2 inhibitor drugs to help people with varying stages of kidney disease. As background, SGLT-2s are a class of drug used to help manage blood glucose levels in people with type 2 diabetes – they reduce A1C, increase time in range, reduce hypoglycemia, and support weigh losst. While metformin is a good option for people with diabetes, for people at risk of kidney disease it makes sense to discuss SGLT-2s with your healthcare professional. Not all SGLT-2s are covered by insurance, but Medicaid, Medicare, and some commercial insurance plans cover select drugs in this class.
Three SGLT-2 inhibitor drugs – Invokana, Farxiga, and Jardiance – have been approved by the FDA for more than glucose lowering: they all reduce risk of heart disease and Invokana is approved treat kidney disease. Jardiance and Farxiga are currently being studied for kidney protection. Cross pointed out that in comparison to GLP-1 agonist medications (another glucose-lowering drug for people with type 2 diabetes), SGLT-2s are preferable for people with kidney disease. Cross concluded that in addition to metformin, SGLT-2s should be considered as an early treatment option for people with diabetes and kidney damage.
If you have diabetes, ask your healthcare team what diabetes management medications might be able to help you protect your heart and kidneys. If you have kidney disease or heart disease, ask whether SGLT-2 inhibitors and GLP-1 agonists could improve your health.
A Pharmacist-Led Collaborative Care Model Improved Health Metrics for People with Type 2 Diabetes
A study conducted at the Crossover Healthcare Ministry compared health outcomes for people with type 2 diabetes in a collaborative care environment, which included pharmacist-led diabetes intensive care visits, and a standard care environment. At the collaborative care clinic, people with an A1C above 9% were directed to a pharmacist and given full support to help manage their risk factors for cardiovascular disease, in addition to standard care practices. Once they met their health goals, they continued long-term care with a primary care physician. The study population was predominantly Hispanic and uninsured.
The study found that people with type 2 diabetes were significantly more likely to meet health goals for blood pressure (under 130/80 mmHg) and LDL cholesterol (below 100 mg/dl) in the collaborative care model, where they worked with a range of healthcare professionals. Likely due to the difference in baseline A1C, the standard care group showed the strongest improvements in A1C. However, this ultimately showed that a collaborative care model – with the addition of a pharmacist to the primary-care team – improved health in people with diabetes. While randomized controlled trials are needed to confirm these results, this initial study indicates that collaborative care models could be helpful for people with diabetes, especially in high-risk populations.
To learn about other health collaborations in diabetes care, click here. If you think you might benefit from talking with a pharmacist, or another specialist, like a heart or kidney professional, or a mental health specialist or a nutritionist, ask your primary healthcare professional if they can refer you.
We’ll be back with more from ADCES20 on health equity, technology, and food – stay tuned for more learning, discussion, and perspective from this ambitious association.









