Zoning in on Sick Day Management: Practical Tips, Strategies, and Advice
By Francine Kaufman
 Pediatric endocrinologist Dr. Fran Kaufman shares tips for managing illness and diabetes: make a sick day plan, have supplies on hand, log your data, modify your insulin doses, and call your healthcare team.
Pediatric endocrinologist Dr. Fran Kaufman shares tips for managing illness and diabetes: make a sick day plan, have supplies on hand, log your data, modify your insulin doses, and call your healthcare team.
Everyone with diabetes who takes insulin needs to have a sick day plan. This is something you develop with your healthcare professional to help you manage the high and low sugar levels that can be associated with an illness. The following advice applies to people with type 1 diabetes and people with type 2 diabetes who take insulin – the advice may be different if you have type 2 diabetes and do not take insulin.
Click to jump down to a section:
When you get sick, you are at risk of becoming dehydrated from poor intake or from excessive loss of fluids due to nausea, vomiting, diarrhea, and fever (your body may lose more water when you have a high temperature). In addition, dehydration is common in diabetes because high glucose levels (above 180-200 mg/dL) cause sugar to enter your urine, dragging an excess amount of fluid with it. Illness also puts you at risk of developing ketones, which when coupled with high glucose levels can lead to diabetic ketoacidosis (DKA), a very serious condition. How do you know if you have ketones? Good question, click here!
The purpose of your sick day plan is to try to keep your glucose levels in a safe range – to avoid dehydration and to prevent ketones from rising to a dangerous level. When you get sick, you should contact your healthcare team to describe your symptoms, determine if they want to evaluate you or send you to a lab (for testing), and most important, to share the numbers that you will collect as you fill in your sick day log (more on this below). It is possible that no matter what you do, you might need to go to an emergency department or be hospitalized – but acting quickly, obtaining the right data, and doing your best to manage your glucose and hydration will minimize risks.
So what illnesses are we talking about? It turns out just about any common bacterial or viral infection – such as the flu (influenza), a cold (upper respiratory virus), tonsillitis, strep throat, an ear infection, stomach flu (gastroenteritis), a bladder infection, and even a skin infection, such as an abscess – can interfere with your diabetes management. However, right now, the greatest concern is COVID-19. An infection with COVID-19 can lead to very high glucose and ketone levels, putting someone at risk for DKA. Acting quickly to start your sick day plan, even if you end up needing to be hospitalized, is important.
When you get sick, your body needs energy to fight the infection and repair damaged tissue. The infections listed above, particularly those that lead to vomiting, diarrhea, fever, and dehydration, cause your body to release certain hormones (called stress or counterregulatory hormones) that tell your liver to release stored glucose and tell your fat cells to release free fatty acids that form ketones. In someone without diabetes, the body releases more insulin to control the rise in glucose and ketones; because you have diabetes, you have to take additional insulin to manage the high glucose and ketone levels. You want to get your sugar levels between 100-180 mg/dL. Blood sugars below 180 mg/dL will prevent excess urination that can dehydrate your body. Staying above 100 mg/dL helps keep you from dipping too low and risking severe hypoglycemia.
If your glucose level is above 180 mg/dL, you need to consider increasing basal insulin doses, using an increase in basal insulin with the temp basal feature on your insulin pump, or giving repeated corrections of bolus insulin with a syringe, pen or pump. Usually, correction doses should not be given more often than every two to three hours to avoid “stacking” insulin, which could lead to low blood sugars. By having a plan for illnesses that starts your modified care early and by keeping in touch with your healthcare team, you are more likely to keep your glucose values in the 100-180 mg/dL range.
But you also have to be concerned about hypoglycemia. Low sugar occurs, particularly in children and the elderly, if the illness affects calorie and carbohydrate intake by decreasing appetite or by causing vomiting or diarrhea. Although low glucose is usually considered to be less than 70 mg/dL, during illness there is concern if glucose levels are below 100 mg/dL. If your infection or illness leads to low glucose levels, reducing basal insulin and not taking bolus insulin doses should be considered. If suspension of insulin is required, you should not suspend or delay taking the next dose of basal insulin for more than 60 minutes, because this increases your risk of developing ketones. Start sipping a sugar-containing drink, one tablespoon at a time. If hypoglycemia continues and you cannot make it better by ingesting sugar, consider the administration of low-dose glucagon. Low-dose glucagon can increase glucose level by 50-200 mg/dL in 30 minutes. To learn about whether low-dose glucagon is right for you, and at what dose, talk with your healthcare team.
To follow what is happening in your body, it helps to start a log of your glucose levels, ketones, fluid intake, and insulin doses. This sick log can be shared with your health care team. It should show improvement from one time period to the next (see below). Note: the biggest concern is vomiting; if you vomit more than twice in a time period or across two time periods, call your healthcare team.
The log shows only two days, because you should be better after 24 hours and completely on the mend after 48 hours. If you are not getting better, call your healthcare team.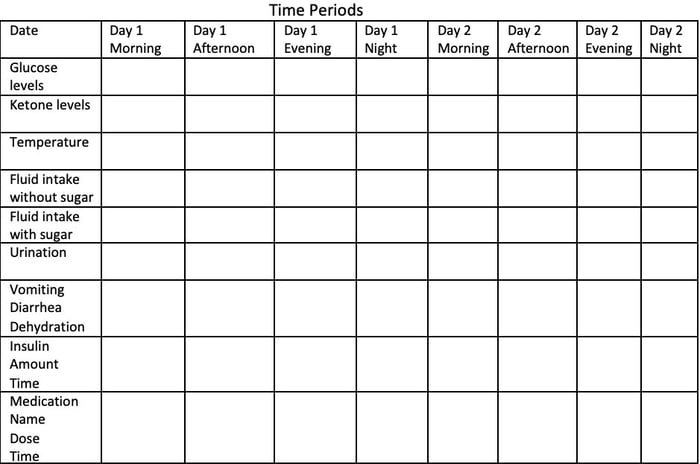 Here’s how to keep track (and why to keep track!) of these important numbers:
Here’s how to keep track (and why to keep track!) of these important numbers:
1. Glucose Levels: Check glucose levels every 1-2 hours. You may have to change this and check your glucose every 30 minutes if your levels are changing quickly. CGM trend data should be looked at every 10-15 minutes. Watch for rapid changes by looking at numbers and arrows. The goal is to keep your glucose between 100-180 mg/dL and without wide swings in values.
2. Ketone Levels: Urine ketones are often detected using a urine ketone strip. A small patch on the strip changes color depending on your level of ketones, representing negative, small, moderate, large and very large levels of ketones. Moderate, large, and very large levels are of concern. Ketones can also be measured with a fingerstick and a special ketone meter. The readings for blood ketones are more accurate and range from 0.0 to 3.0 mmol/L or greater. Blood ketone levels below 0.6 mmol/L are considered normal. Between 0.6 and 1.5 mmol/L ketones are high and show that your fat has broken down to form excess ketones. This puts you at risk of DKA if glucose levels are also elevated. Ketone levels above 1.5 mmol/L are serious, and you should contact your healthcare professional. Signs of elevated ketones:
-
Nausea and vomiting (which may also be present because of the infection)
-
Shortness of breath and labored breathing (your body is trying to eliminate the ketones through your breath so you can also smell them, they make your breath smell fruity)
-
Weakness
-
Altered level of consciousness and trouble staying awake (this is most concerning; call your healthcare professional immediately if this is happening)
Ketones should be tested at the onset of an illness and then every four hours. If ketone and glucose levels are both elevated, your healthcare team might advise you to increase correction insulin doses further, by an additional 10-15%. If ketone levels are high and glucose levels are not high (less than 150 mg/dL), oral glucose and some insulin – reduced by about 50% – will help clear your ketones. Drinking water will also help reduce ketones as they are removed in the urine. To learn more about ketones, including what they are and how to measure them, click here.
3. Temperature: High fever can help show the severity of your illness, particularly if it is persistent. We have learned that COVID-19 is associated with persistent high fever. Use the log sheet to document any medications you take to lower fever so that you can report this to your healthcare team.
4. Fluid Intake, with and without Sugar: Consuming liquids is critical if there is risk of dehydration. Fluids with sugar should be taken if glucose levels are between 100-150 mg/dL, and fluids without sugar should be taken if glucose levels are between 150-180 mg/dL. If you have vomited, wait 30-60 minutes before trying to drink, and then start with teaspoons of water or ice chips, progressing to tablespoons and ounces. The goal is to retain 4-6 ounces of fluids (or 2-4 ounces for young children) every 30-60 minutes until you can drink without risk of vomiting and as your thirst dictates. Food is much less important after vomiting; don’t try to eat food until you are on the mend.
5. Urination: Noting frequency and amount (small, medium, or large) is important to understand the ongoing risk of dehydration. As glucose levels reach the target of 100-180 mg/dL, you should see a decrease in both frequency and amount of urination, as well as less dehydration.
6. Vomiting, Diarrhea and Dehydration: Vomiting and diarrhea can lead to dehydration. The signs of dehydration include dry mouth, sunken eyes, weakness, loose skin, rapid heart rate, and low blood pressure. Vomiting is also of great concern because it occurs not only from the illness, but as a result of DKA. That’s why vomiting that occurs throughout one time period or spans two time periods in your log means it is time to call your healthcare professional. However, if you feel weak after vomiting only once or twice, it is always better to call earlier than later.
7. Insulin, Amount and Time: One of the most important things to remember is that during an illness, you still need to take insulin. Even if you are not eating or drinking at the beginning, you need to have insulin in your body. Insulin allows sugar to enter your body’s cells to be used for energy, and you need more energy to fight off an illness. Insulin also reduces ketone formation and stops excess urination by lowering glucose levels. If you have high glucose, you might need 25-50% more insulin than you usually take, due to insulin resistance created by the extra stress or counterregulatory hormones in your body. If you have low glucose, you might need to take 25-50% less insulin than you usually take, but you still need some basal or background insulin on board.
8. Medications: At the beginning of an illness, you should consider calling your healthcare team to determine if you should avoid taking any of your routine medications while sick. This includes glucose-lowering pills or injections, such as SGLT-2 and GLP-1 drugs, or medications for blood pressure and cholesterol. In addition, it is important to write down any medications you take (name, dosage, time) to treat fever, vomiting, diarrhea, or other symptoms of your illness. Anti-vomiting medications may be helpful but should only be taken after discussing with your healthcare professional.
-
Know your sick day plan before you become sick.
-
Have supplies on hand. These include supplies to measure glucose, a way to measure ketones, a thermometer, sugar-containing fluids, glucagon, extra-rapid (or short) acting insulin, and medication to treat fever. Discuss with your healthcare team whether you should have medication for diarrhea and vomiting on hand.
-
Have all the contact information for your healthcare team available, and call them sooner rather than later.
-
Before you call your healthcare team, have the data listed on your log sheet written down, plus your symptoms.
-
Take insulin at modified doses to address both high and low glucose levels. You still need to have some insulin in your body, even if you are not eating.
-
Let someone help you while you are ill. It is too big a job to be done alone.
About Fran
Dr. Fran Kaufman is the Chief Medical Officer of Senseonics, Inc. She is a Distinguished Professor Emerita of Pediatrics and Communications at the Keck School of Medicine and the Annenberg School of Communications at the University of Southern California.







